Shoulder replacement surgery is a game-changing solution for painful arthritis of the shoulder. Continued advancements in orthopedic knowledge and experience with shoulder replacements have led to improved technologies...
Shoulder replacement surgery is a game-changing solution for painful arthritis of the shoulder. Continued advancements in orthopedic knowledge and experience with shoulder replacements have led to improved technologies, surgical techniques, and better surgical outcomes.
Shoulder arthritis is an extremely common cause of shoulder pain in the over 50 population. Most frequently, it is a result of wear and tear (osteoarthritis) over the years. It can also follow traumatic injuries, recurrent shoulder instability, massive rotator cuff tears, rheumatoid arthritis, and other medical conditions.
In the healthy state, the shoulder’s joint surfaces are covered with a thin layer of cartilage that provides for a smooth, nearly frictionless pain-free motion (Figure 1). As the cartilage becomes worn over time, the cartilage softens and breaks down leading to arthritis. Arthritis is diagnosed with x-rays demonstrating bone spurs, narrowing of the space between the joint surfaces, thickening of the bone beneath the diseased cartilage, and cysts within the bone (Figure 2).

Figure 1. X-ray of a normal shoulder.
There is a wide and congruent joint space between the humeral head (ball) and the glenoid (socket). This space is occupied by the cartilage cap of the two joint surfaces, and this is cartilage is not directly visible on an x-ray. Note the smooth contour of the two joint surfaces.

Figure 2. X-ray of a severely arthritic shoulder joint.
Figure 2. X-ray of a severely arthritic shoulder joint. Note the bone-on-bone contact of the humeral head on the glenoid. Also there are large bone spurs and increased density of the bone beneath the diseased cartilage called sclerosis (more intense white appearance of the bone).
The signs and symptoms of shoulder arthritis include pain with activities, pain during sleep, a grinding or popping feeling with motion, and stiffness. As a progressive disease, it tends to worsen over time.
Early treatment of shoulder arthritis pain often includes use of non-steroidal anti-inflammatory drugs (NSAIDs), activity modification, and sometimes physical therapy. A cortisone injection can also be a potent pain reliever, but there is really no way to predict how long or how much it will help before you try. Unfortunately, these pain-relieving options do not change the course of this progressive disease and inevitably they will no longer be effective in controlling the pain.
Many individuals will reach a point where these pain-relieving treatments are no longer effective, and a shoulder replacement will be the next step. Shoulder replacement surgery is a safe and effective procedure to relieve pain, maintain or improve motion, and return to routine activities and sports such as golf and tennis.
You may benefit from a shoulder replacement if you have severe pain with daily activities, stiffness, weakness, or pain interfering with sleep.
If you are suffering from these symptoms, you should see a shoulder replacement specialist for a thorough evaluation. This will involve a review of your symptoms and prior treatments, a physical examination of your shoulder, x-rays, and sometimes additional testing such as a CT scan or MRI. Recommendations can then be given as to whether shoulder replacement surgery is right for you.
Shoulder replacements are very similar to hip and knee replacements, and have a proven track record of high patient satisfaction and excellent longevity in the current orthopedic literature. The diseased arthritic joint surfaces are replaced with highly polished metallic and medical-grade polyethylene implants.
There are two main types of shoulder replacements: anatomic total shoulder replacement and reverse total shoulder replacement. The type of implant chosen is generally based on the condition of the shoulder’s rotator cuff.
If the rotator cuff is healthy, we implant an anatomic total shoulder replacement, whose components resemble the natural contours of the native joint surfaces (Figure 3).

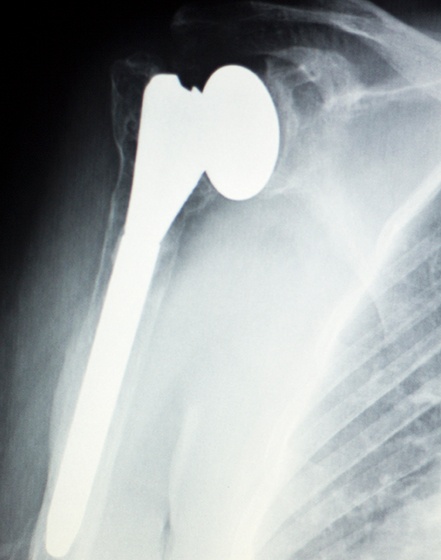
Figure 3. Anatomic total shoulder replacement.
Note the replacement of the humeral head with a smooth hemispherical ball that attaches to a metal stem that sits inside the humerus (arm bone). On the glenoid side, there is a newly resurfaced socket made of polyethylene (plastic).
If the rotator cuff is in poor condition, a reverse total shoulder replacement is implanted. The ball-and-socket of this type of replacement is reversed from the native anatomy. This type of prosthesis was developed to allow for the shoulder’s deltoid muscle to provide the power to move the shoulder without the help of the damaged rotator cuff.
When undergoing an operation, individuals often are concerned about the pain of surgery and the time frame of recovery.
First, I have found that postoperative pain can be greatly diminished with a thoughtful plan for pain management utilizing a specific protocol I’ve developed including preoperative counseling, intraoperative anesthesia techniques, gentle handling of the shoulder during surgery, and use of a combination of postoperative prescription medicines.
With my current protocol, some patients are now candidates for shoulder replacement on an outpatient basis at a state of the art surgical center in Palm Beach Gardens, FL. My patients who have had surgery as an outpatient procedure have definitely been some of my happiest and most satisfied.
For other individuals, the procedure is done in the hospital and they go home one to two days postoperatively.
The ultimate success of the operation is greatly affected by your cooperation in following the surgeon’s instructions after surgery. The wound should be kept clean and dry until the skin incision is sealed. You should avoid lifting anything heavier than a glass of water for the first 4 weeks. A sling is worn for 6 weeks to protect the shoulder during the early healing phase, at all times except for showering and during your prescribed home exercises. Within a few days of surgery, a physical therapy program is started and generally continues for 8-12 weeks. By 3 months postoperatively, you can return to activities such as golf. In order to extend the longevity of the shoulder replacement, avoid contact sports and heavy lifting.
Shoulder replacement surgery can really improve one’s quality of life and is an excellent solution for shoulder arthritis pain when other measures fail. When deciding whether a shoulder replacement might be right for you, seek the care of a shoulder surgeon you have confidence in and can trust.





